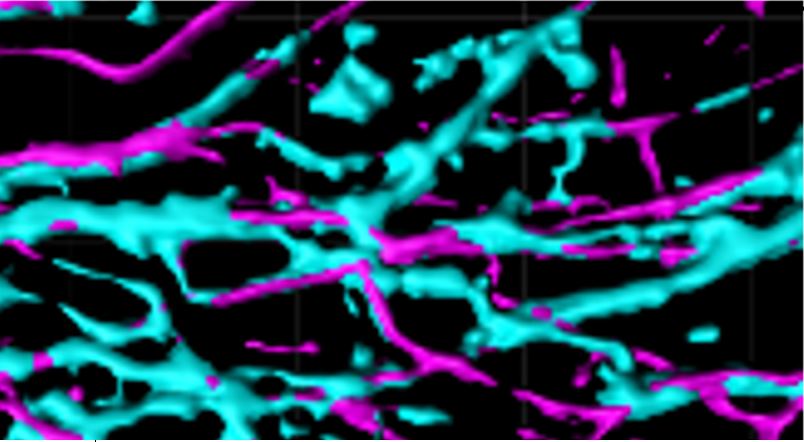
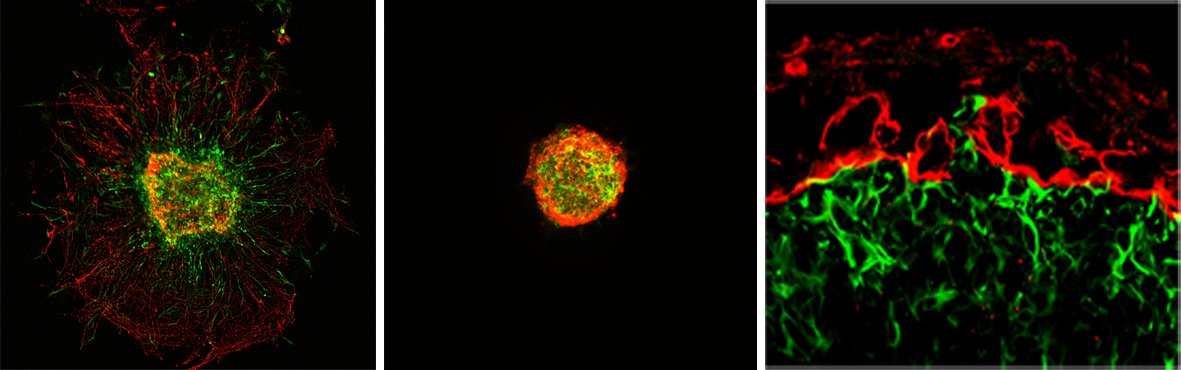
Central Nervous System (CNS) Myelination
Myelin is a specialized multilamellar membrane structure that is formed by oligodendrocytes (OLs) of the CNS. OLs follow an orderly and distinct developmental pattern with stage-specific functions, including OL precursor cell (OPC) proliferation, pre-myelinating OL (pmOL) ensheathment of axons, and myelinating OL (mOL) iterative wrapping of axons. Cytoskeletal rearrangements play an important but different role at each stage. Actin filament (F-actin) formation is essential for axon ensheathment in pmOLs, whereas F-actin disassembly is required for mOL sto wrap axons. Ongoing research efforts aim to elucidate molecular mechanisms underlying pmOL biology, axon ensheathment, and their implications in myelin-related diseases, including developmental white matter injury and multiple sclerosis.
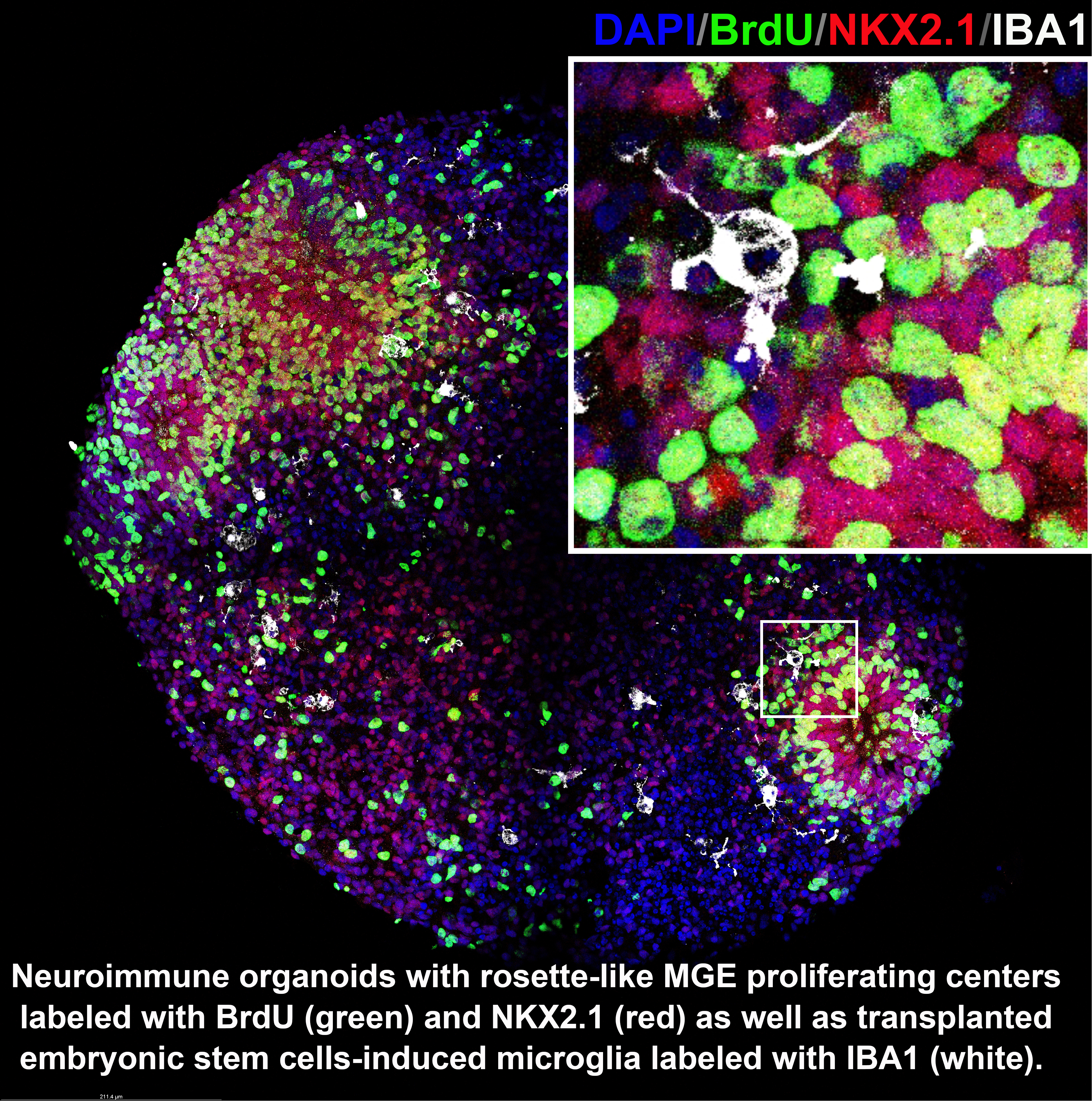
Neuro-immune interplays during interneuron development
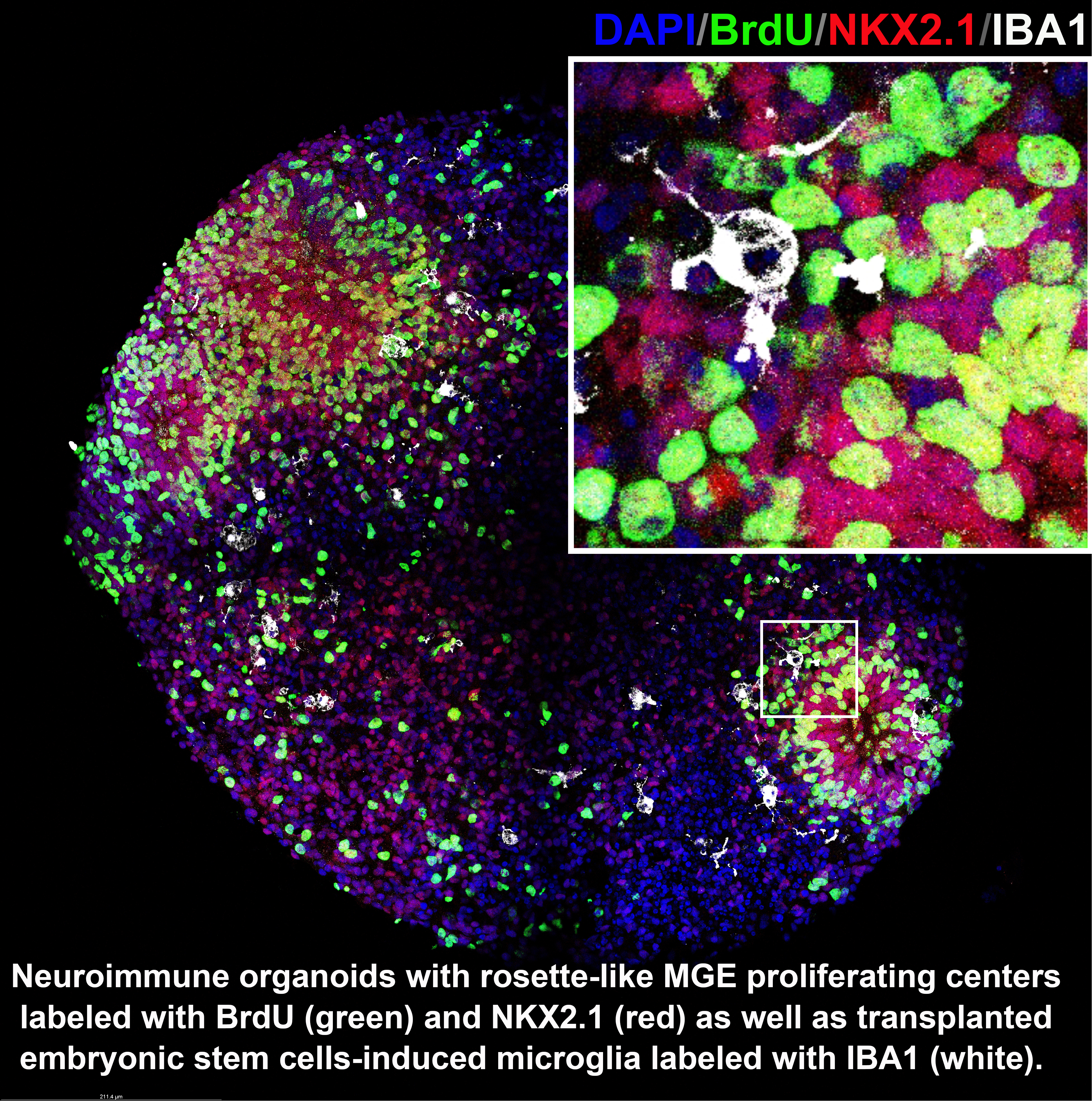
Cortical interneurons provide the main cortical inhibitory input and play a critical role in maintaining circuit rhythm and excitation-inhibition balance in the brain. Their deficits have been implicated in multiple neurological disorders, including autism spectrum disorders, epilepsy, and schizophrenia. Our understanding of how neuroimmune interaction contributes to interneuron development is primitive and does not, so far, enable a precision medicine approach. Until recently, existing technology was inadequate to decipher interactions that underlie neuroimmune processes. With the advent of genome-wide data analysis, organoids, and deep perturbation biology, along with artificial intelligence/machine learning and related data science, it is now feasible to tackle these complex questions. By leveraging these recent technological advances, we are taking innovative multidisciplinary approaches to attack this exceedingly challenging problem. Its success will accelerate the decoding of the many brain diseases in which the immune system is implicated.
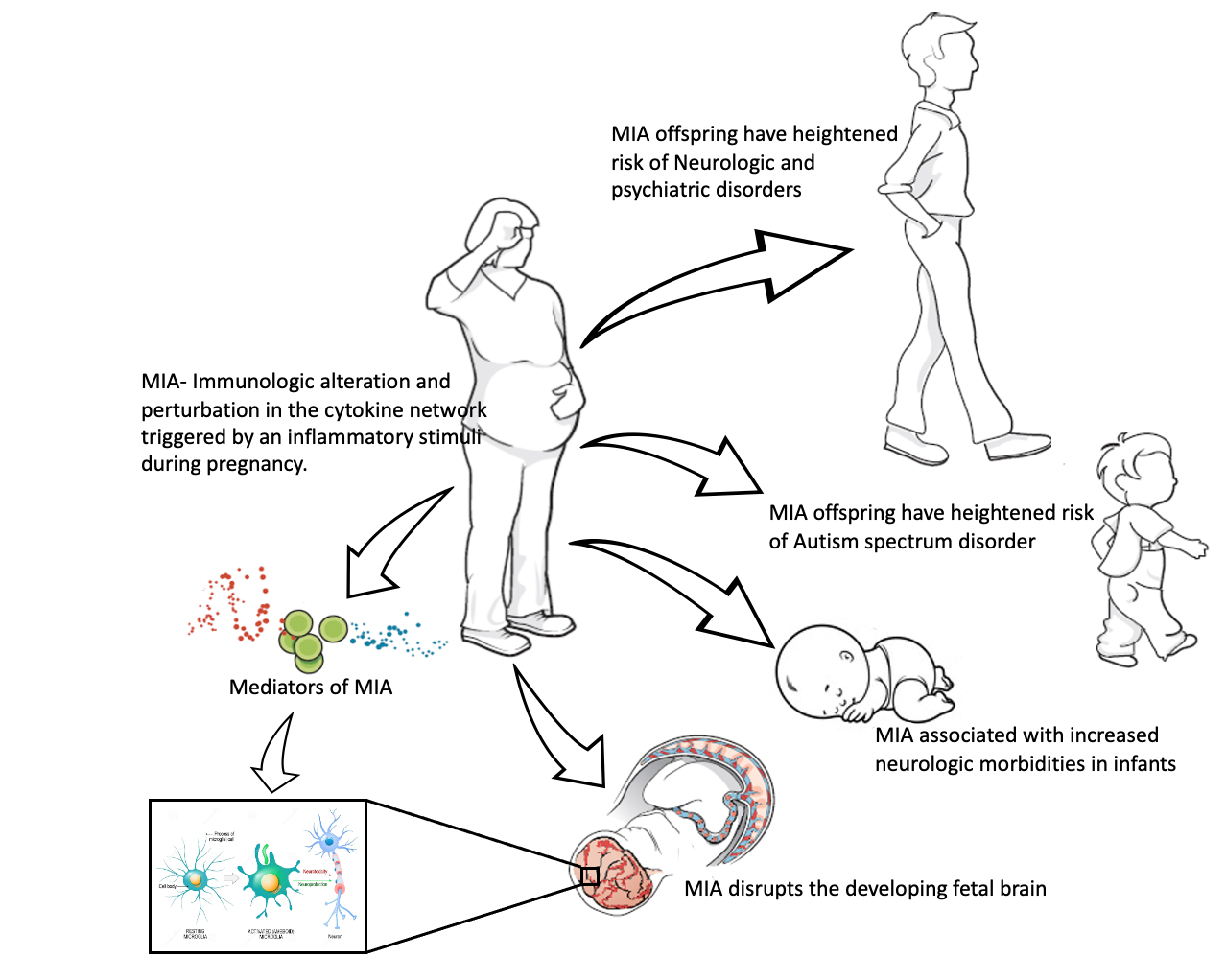
The impact of maternal immune activation on brain development
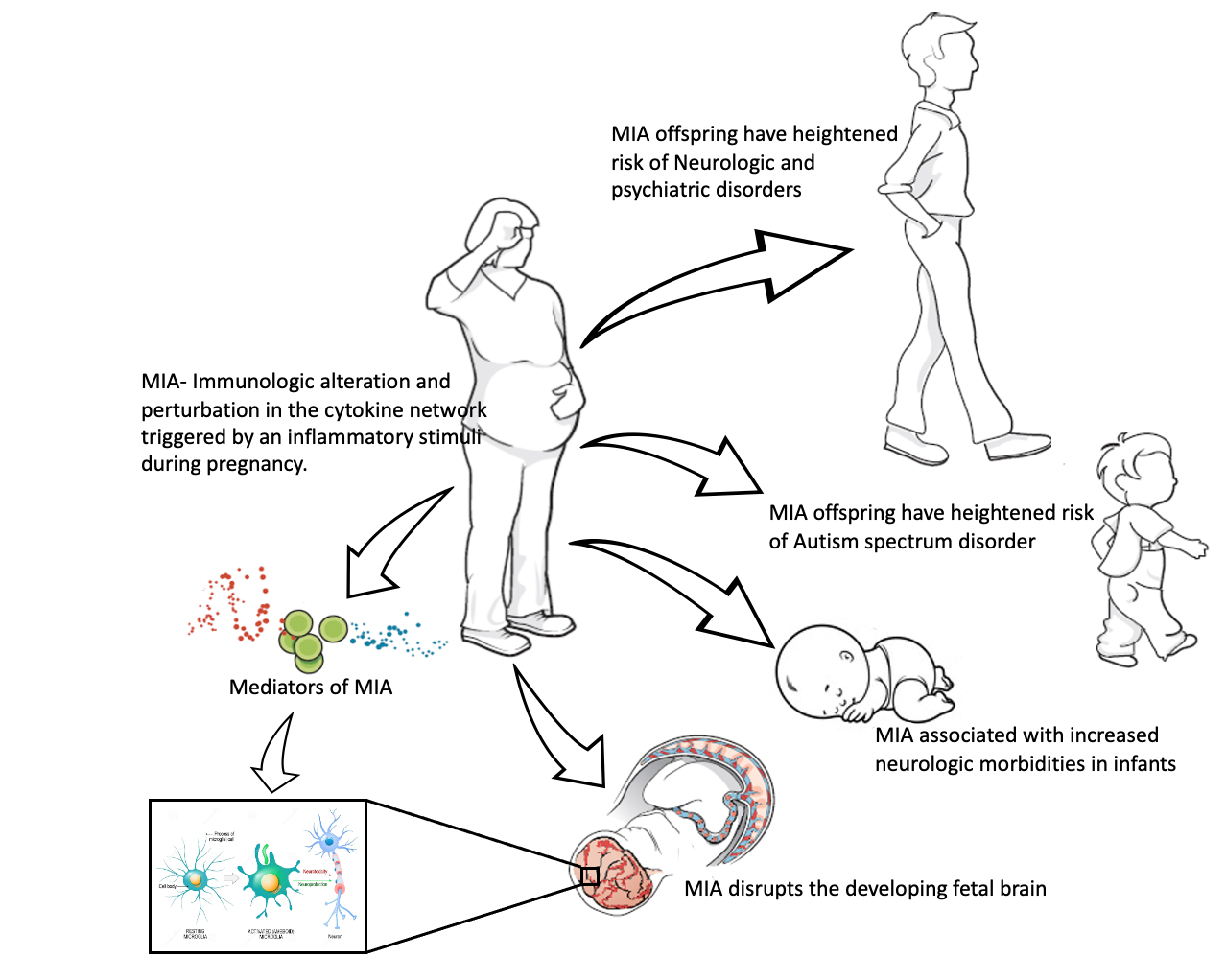
Maternal immune activation (MIA) can be defined as an immunological alteration triggered by an inflammatory stimulus during pregnancy. Epidemiological and animal model studies have found MIA to be associated with neuropsychiatric disorders in offspring like autism spectrum disorders, attention deficit hyperactivity disorder (ADHD), and schizophrenia. Additionally, results from our epidemiological study found MIA to be associated with neurological morbidities in offspring, such as periventricular leukomalacia (PVL), seizures, and abnormal neurological exams, as early as the neonatal period. These results suggest a disruption in the fetal neurodevelopmental processes secondary to MIA. However, the mechanisms through which MIA perpetuates its impact remain poorly understood. Utilizing translational research techniques, we plan to identify the specific mediators of MIA that create these neurodevelopmental morbidities in offspring. Ongoing research aims to uncover the cellular and molecular mechanisms underlying MIA-mediated neurodevelopmental disruption. Such an understanding will provide therapeutic and preventative opportunities to mitigate the most detrimental impacts of MIA on the developing fetal brain.
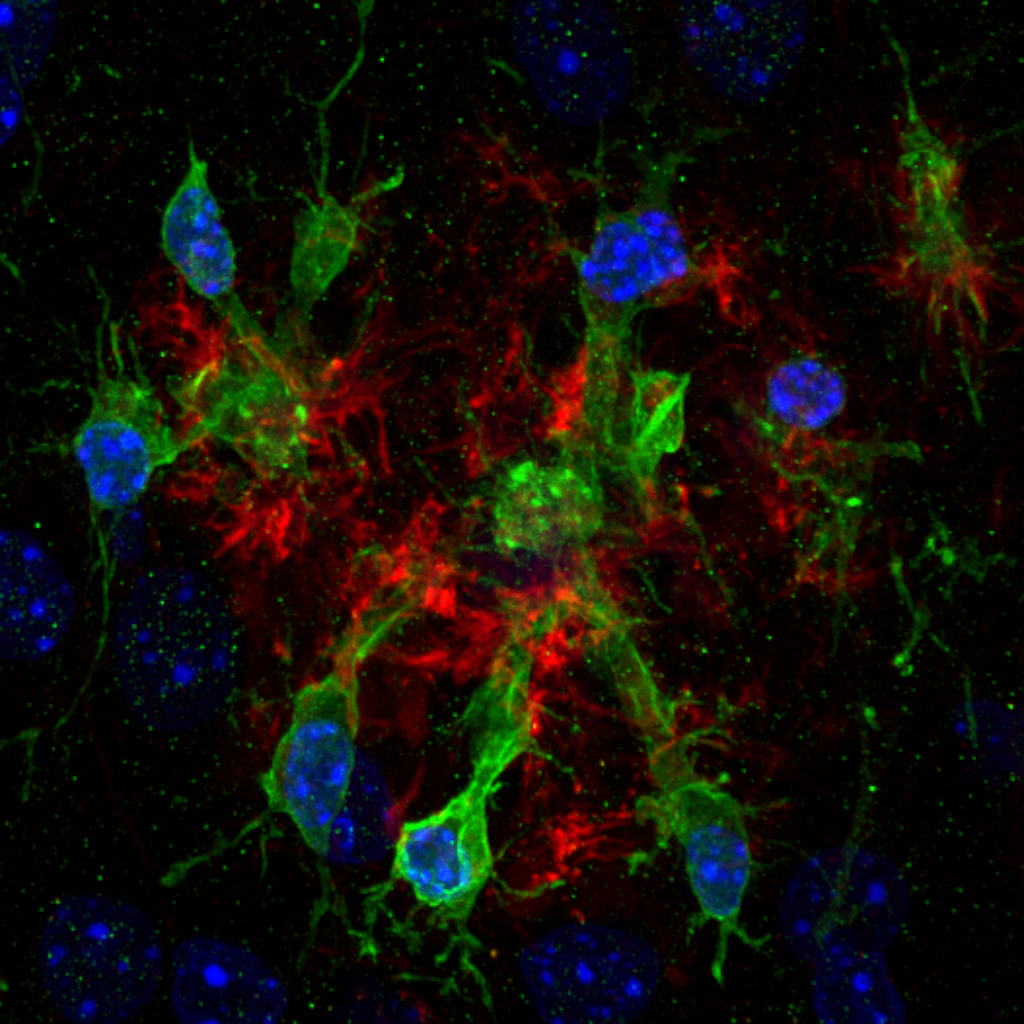
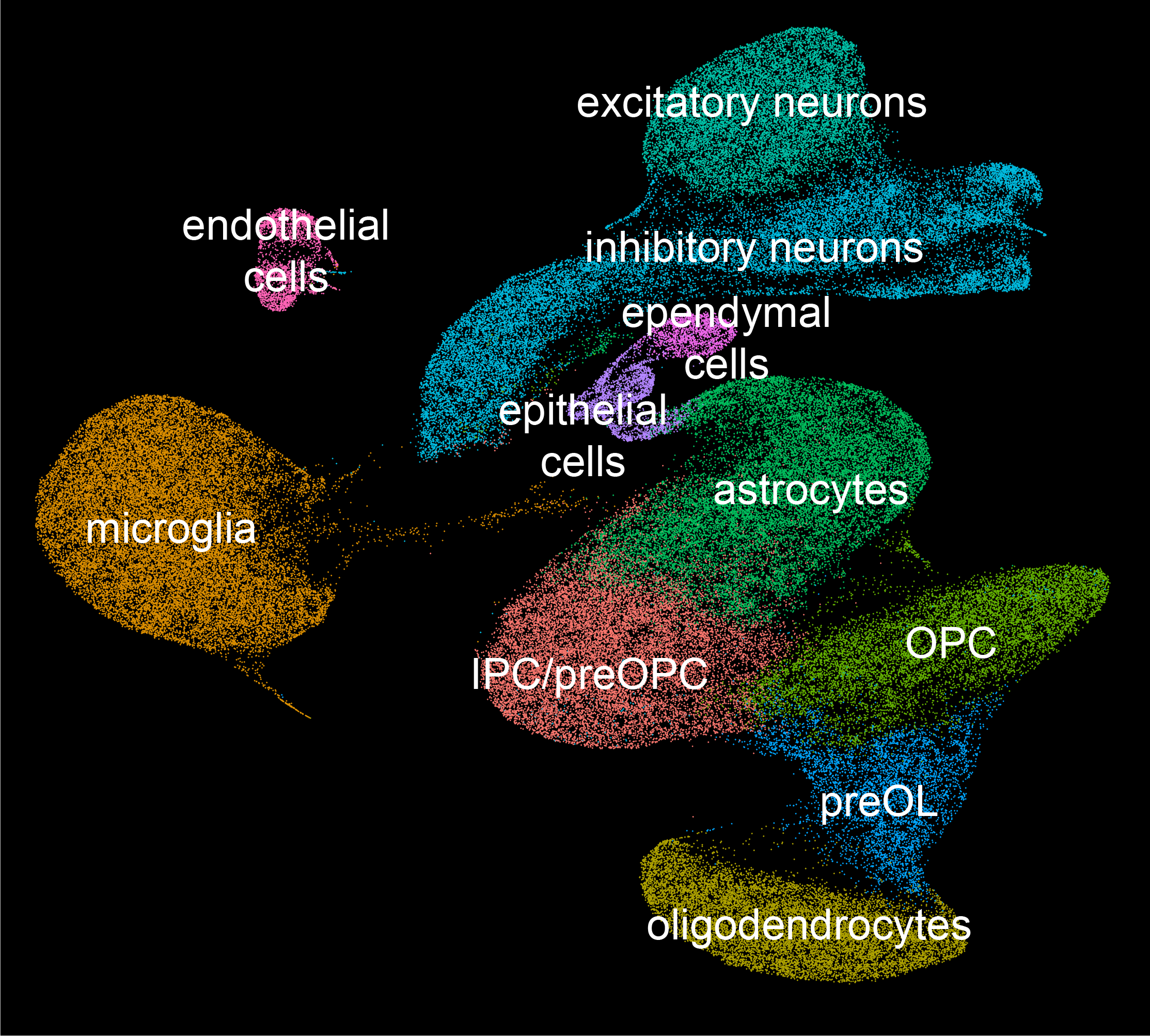
Glial-glial and glial-neuronal interactions in Alzheimer's disease
Glial cells play key functions during brain homeostasis and their dysfunction contributes to neurodegeneration such as Alzheimer's disease (AD). Our ongoing research investigates glial contributions to AD pathology. We generated single-nucleus RNA-sequencing (snRNA-seq) datasets in mouse transgenic models. Additionally, our lab is planning on generating snRNA-seq datasets for brain samples from post-mortem humans with AD. Previously published computational algorithms on inferring cell-cell interactions between different cell types will be used to identify and evaluate the glial interactions responsible for AD development. We also plan on utilizing spatial transcriptomic profiling methods to identify local cell-cell interactions.